at Kalmar Family Podiatry in Huntington, NY
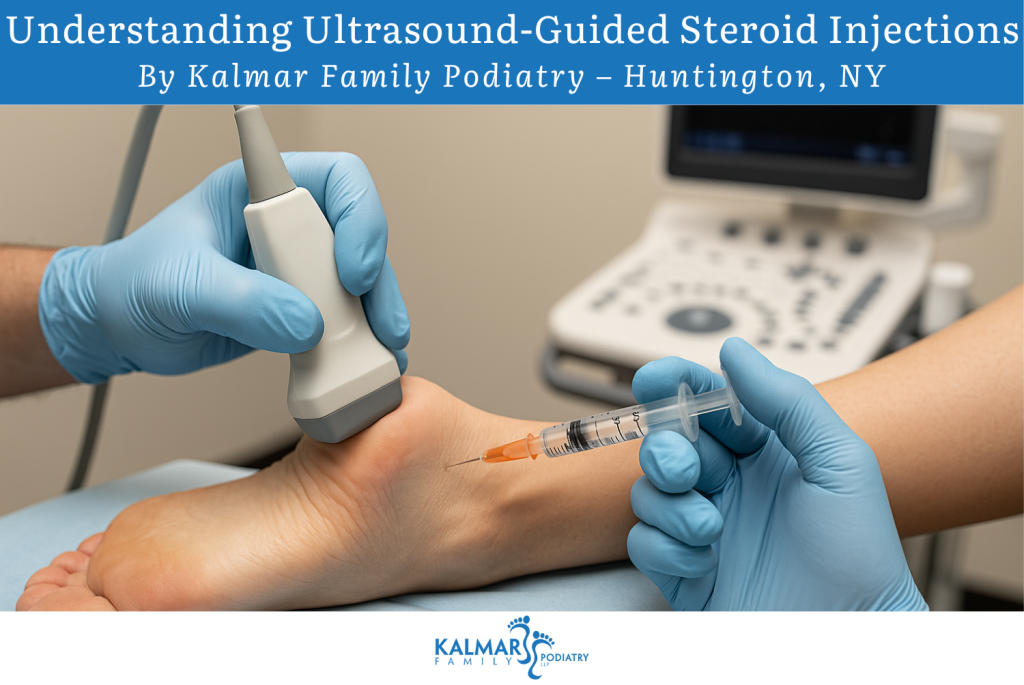
At Kalmar Family Podiatry, we are committed to providing state-of-the-art treatments for foot and ankle pain. One of the advanced techniques we offer is ultrasound-guided steroid (corticosteroid) injections, which allows us to deliver effective relief in a precise, safe, and minimally invasive manner.
Below is a comprehensive guide to how this treatment works, why it’s beneficial, when it’s appropriate, what to expect, and a Q&A section to help you make informed decisions.
What Are Ultrasound-Guided Steroid Injections?
An ultrasound-guided steroid injection is a medical procedure in which a corticosteroid (plus often a local anesthetic) is injected directly into or around an area of inflammation (such as a joint, tendon sheath, or bursa) while using real-time ultrasound imaging to guide the needle to the exact target. The ultrasound allows visualization of bones, soft tissues, tendons, nerves, and blood vessels, helping avoid structures that should not be punctured. PMC+2podimedic+2
In podiatric (foot and ankle) practice, these injections are used to treat conditions like plantar fasciitis, tendon inflammation, Morton’s neuroma, joint arthritis, bursitis, and more. PMC+2podimedic+2
Why Use Ultrasound Guidance?
1. Precision & Accuracy
Ultrasound guidance enables the podiatrist to see exactly where the needle is going, rather than relying only on anatomical landmarks. This typically leads to greater accuracy in placing the medication in the ideal spot. PMC+2podimedic+2
Studies have shown that ultrasound-guided injections in the foot and ankle have high success rates for symptom relief. PubMed+1
2. Reduced Risk of Complications
By visualizing surrounding structures in real time, the risk of inadvertently injuring nerves, vessels, tendons, or cartilage is reduced. UCSF Radiology+1
3. Better Outcomes
Because the medication is delivered exactly where needed, many patients experience faster and more effective relief than with “blind” injections. podimedic+2HMP Global Learning Network+2
4. Non-Radiative, Real Time, Flexible
Unlike fluoroscopy (X-ray guidance), ultrasound uses no ionizing radiation and offers dynamic, real-time imaging of soft tissues. UCSF Radiology+1
Common Foot & Ankle Conditions Treated with This Technique
Ultrasound-guided steroid injections are used in numerous podiatric settings. Some of the more common conditions we address include:
- Plantar fasciitis / plantar heel pain / heel spur syndrome
- Tendonitis / tenosynovitis (e.g., Achilles, peroneal, posterior tibial)
- Bursitis
- Morton’s neuroma or intermetatarsal bursitis
- Arthritis in foot/ankle joints (metatarsophalangeal, midfoot, subtalar, etc.)
- Capsulitis / joint inflammation
- Plantar fibromatosis / nodules in the plantar fascia podimedic+2PMC+2
Ultrasound guidance allows us to access small joints (metatarsophalangeal, tarsometatarsal), tendon sheaths, and anatomical niches that would be difficult or risky to reach without imaging guidance. PMC+2PubMed+2
Procedure: What to Expect
Here’s a step-by-step look at how we perform the injection at Kalmar Family Podiatry:
- Initial Evaluation
- Review of your medical history
- Physical exam, biomechanical assessment
- Imaging or X-rays as needed
- Diagnostic ultrasound scan to observe inflamed areas
- Review of your medical history
- Preparation
- The skin is cleaned and prepped under sterile conditions
- A local anesthetic (such as lidocaine) is often injected first to numb the area
- The ultrasound probe is positioned to visualize the target structure
- The skin is cleaned and prepped under sterile conditions
- Guided Needle Placement
- Under continuous ultrasound visualization, we guide a fine needle (often 23–25 gauge for small structures, larger for deeper or larger joints) into the target area. PMC+1
- The needle trajectory is adjusted in real time to avoid nerves, vessels, and tendons
- Under continuous ultrasound visualization, we guide a fine needle (often 23–25 gauge for small structures, larger for deeper or larger joints) into the target area. PMC+1
- Injection of Medication
- A mixture of corticosteroid and local anesthetic is slowly injected
- We observe the spread of the injection under ultrasound to confirm proper placement
- A mixture of corticosteroid and local anesthetic is slowly injected
- Post-Injection Protocol
- A light dressing or bandage is placed
- You may rest for a short period
- Ice and elevation may be recommended initially
- Avoid strenuous activity for at least 24–48 hours
- Follow-up with physical therapy, stretching, orthotics, or other adjunctive treatments as needed
- A light dressing or bandage is placed
The entire procedure usually takes about 30 to 60 minutes, though much of this is preparation, planning, and post-injection rest. UCSF Radiology+1
Benefits & Limitations
Benefits
- Directly targets the source of inflammation
- Faster onset of relief
- Less collateral tissue irritation
- Avoids systemic side effects of oral steroids
- Excellent safety profile with experienced operators
Limitations & Considerations
- The relief is often temporary (weeks to months)
- Repeated injections in the same anatomic site may weaken tendons or tissues over time
- Steroid injections are not suitable for all patients (e.g., uncontrolled diabetes, infection, bleeding disorders)
- Not all structural damage is reversible; injections are part of a broader management plan
- Some cases may need supplemental therapies (physical therapy, orthotics, surgery)
Recovery & Aftercare
- Rest & offloading: Limit activity on the affected foot for the first 24–48 hours
- Ice & comfort measures: Use ice packs, elevate the foot, and take analgesics as advised
- Gradual return: Reintroduce gentle motion and stretching as pain allows
- Follow-up care: You may be referred for physical therapy, custom orthotics, or further imaging
- Monitoring: If pain worsens or signs of infection (redness, swelling, fever) occur, contact us promptly
Q&A: Everything You Want to Know
Q: Is the injection painful?
A: You may feel a brief sting when the local anesthetic is injected. After numbness, further needle insertion and steroid injection are usually well tolerated. The ultrasound guidance helps minimize repeated punctures, reducing discomfort.
Q: When will I feel relief?
A: Some patients experience pain relief within hours (due to the anesthetic). The anti-inflammatory effect of the steroid typically develops over 2 to 7 days, with maximum benefit in subsequent days or weeks. podimedic+3Wikipedia+3HMP Global Learning Network+3
Q: How long does the relief last?
A: Duration varies by condition, severity, and individual response. Relief may last weeks to months. In some cases, repeat injections may be considered, but typically limited to avoid tissue damage.
Q: How many injections can I have?
A: Usually, we limit to 2–3 injections per site per year, with sufficient intervals between them. Overuse of steroids in a single location can weaken tendons or soft tissues.
Q: Are there side effects or risks?
A: Though rare, potential risks include infection, bleeding, local tissue thinning, nerve irritation, temporary flare in pain, or adverse reactions (especially in patients with diabetes, immunosuppression, or bleeding disorders). Using ultrasound minimizes many of these risks. UCSF Radiology+1
Q: Are there people who shouldn’t get these injections?
A: We may avoid them in patients with active infection, uncontrolled diabetes, bleeding disorders, allergy to steroid ingredients, or poor vascular supply. Each patient is evaluated individually.
Q: Does the injection “mask” pain without treating the cause?
A: The injection addresses inflammation and often helps break the pain-cycle, but underlying mechanical or structural issues (e.g. gait abnormality, foot alignment, overuse) must be addressed through supportive therapies.
Q: How does this compare to PRP or biologic injections?
A: Platelet-rich plasma (PRP) and other biologics aim to promote healing rather than only reduce inflammation. In select cases, we may combine or choose alternative biologic treatments. Ultrasound guidance is often used across these modalities. PMC+2PubMed+2
Q: Can I drive home afterward?
A: Usually yes, although some numbness or discomfort might persist briefly. For lower extremity injections, it’s advisable to have someone accompany you just in case. UCSF Radiology
Q: What should I do to prepare?
A: Wear loose clothing, avoid applying lotions to the injection site, disclose all medications (especially blood thinners), and inform us of any prior reactions or medical conditions.
Why Choose Kalmar Family Podiatry in Huntington, NY?
- We combine specialized foot-and-ankle expertise with advanced imaging capabilities
- Our team is experienced in ultrasound-guided interventions for podiatric conditions
- We provide a holistic plan: injections are just one tool in our broader strategy (orthotics, therapy, gait correction, lifestyle modifications)
- You receive personalized attention and follow-up care to maximize your outcomes
To learn more about our ultrasound-guided injection services or to schedule an appointment, visit our dedicated Ultrasound-Guided Injection at Kalmar Family Podiatry page.
Contact Information
Kalmar Family Podiatry
📍 62 Green Street, Huntington, NY, 11743
📞 (631) 549-0955
🌐 kalmarfamilypodiatry.com
Feel free to contact us with questions or to schedule your consultation. We look forward to helping you step pain-free.
